Data & Reporting
Gain full visibility and actionable insights into your revenue cycle and business performance.
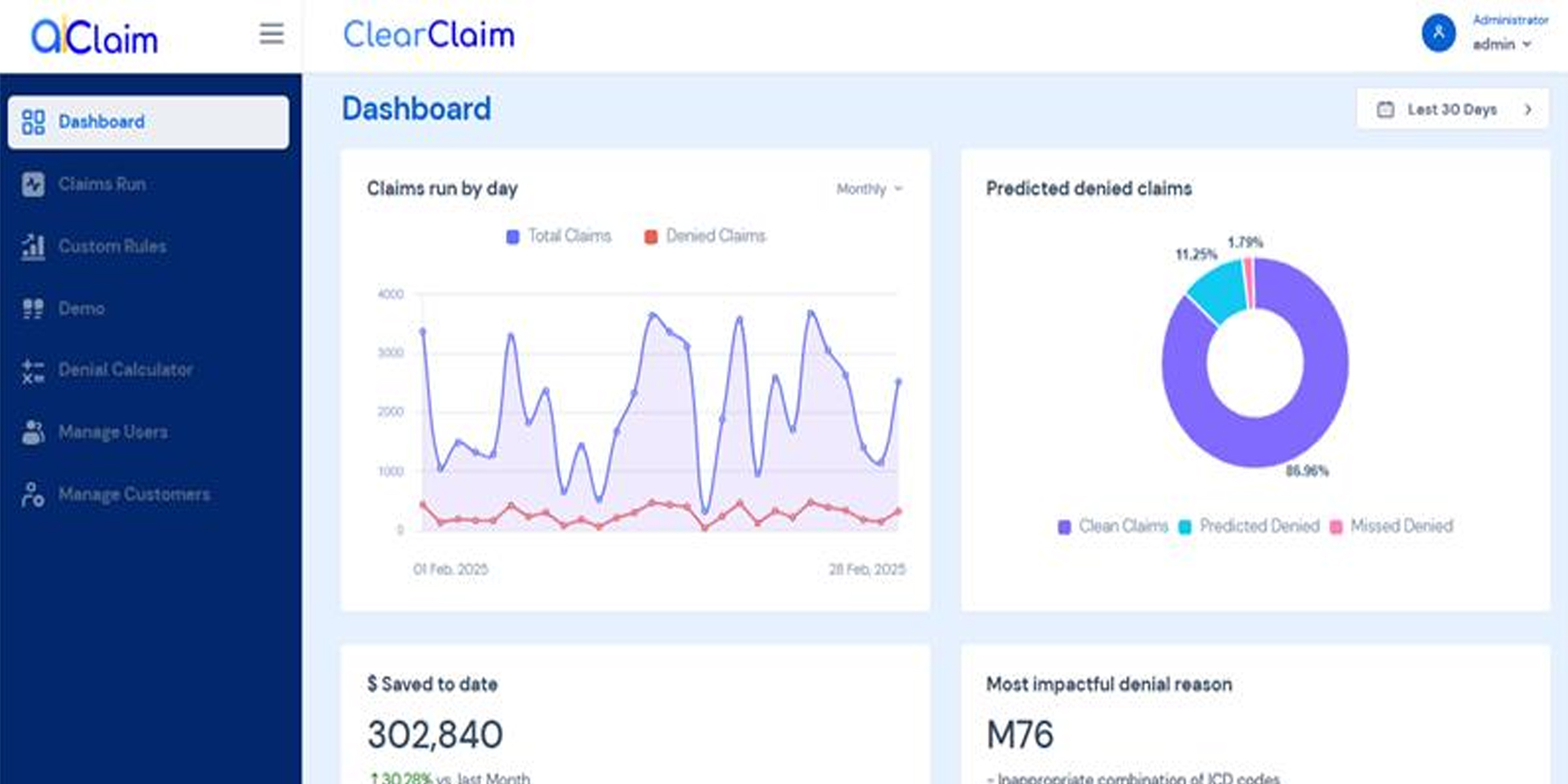
Intelligent claim denial prediction that integrates with your existing workflows
Our advanced AI model delivers industry-leading accuracy to identify potential claim denials before submission.
Integrates with your existing Revenue Cycle Management (RCM) workflows with no disruption to your current systems.
Easy direct processing of standard X12 837 EDI files with zero additional data preparation needed.
Flexible API endpoints for customized integrations with your existing practice management systems.
Identify and fix issues before submission to maximize clean claim rates and minimize revenue cycle time.
Coming soon: AI-powered agents that automatically work up denials to speed resubmission and payment.
Our intelligent platform constantly validates every aspect of your billing—credentialing, provider data, and more. With real-time rules enforcement, your claims are always clean, accurate, and ready for submission.
Our powerful engine automatically detects and corrects inconsistencies in payer requirements, ID mismatches, and contract data—ensuring zero claim rejections due to avoidable errors.
Customize your workflows with ease. Set up personalized credentialing rules, billing logic, and compliance standards directly in our system—giving you full control at scale.
Implement your own coding policies with precision. Automatically hold claims that fail CPT code criteria, ensuring policy compliance before submission.
A modern revenue cycle automation platform designed for growing healthcare practices— streamlining billing, reducing denials, and accelerating payments.
Get a demo today